Migraine headaches: terrible agony for gamers

Key points
Disclaimer
This information is for educational purposes only and is not intended to replace the advice of your doctor. Esports Healthcare disclaims any liability for the decisions you make based on this information.
The information contained on this website does not establish, nor does it imply, doctor-patient relationship. Esports Healthcare does not offer this information for diagnostic purposes. A diagnosis must not be assumed based on the information provided.
What are migraine headaches?
Migraine headaches are true, primary headaches affecting the brain and its surrounding tissues. There are different theories about migraines, but one of the more widely accepted theories describes a phenomenon called cortical spreading depression.
Note: This information is based on a well-researched theory. This theory is currently the best available. As new research is published, this information will be updated and changed, if necessary.
Pathophysiology: theory of cortical spreading depression
It is described that migraine headaches occur following a particular trigger. These triggers may include coming in contact with an allergen, certain ingredients in food, physical or psychological stress, weather patterns, lack of sleep, etc. Ultimately, the triggers are still not widely understood, and researchers have been unable to confirm specific causes for the initial onset of migraine headaches.
In the model of cortical spreading depression (CSD), a wave of depolarization (or activation of a nerve) spreads across the cortex of the brain following the trigger of a migraine headache.
Note: the cortex of the brain is where all conscious activity occurs, including conscious thought, speech, motor control, and sensory input.
Following this wave of depolarization, brain activity becomes mildly depressed. In other words, the nerves become somewhat inhibited and electrical activity is decreased.
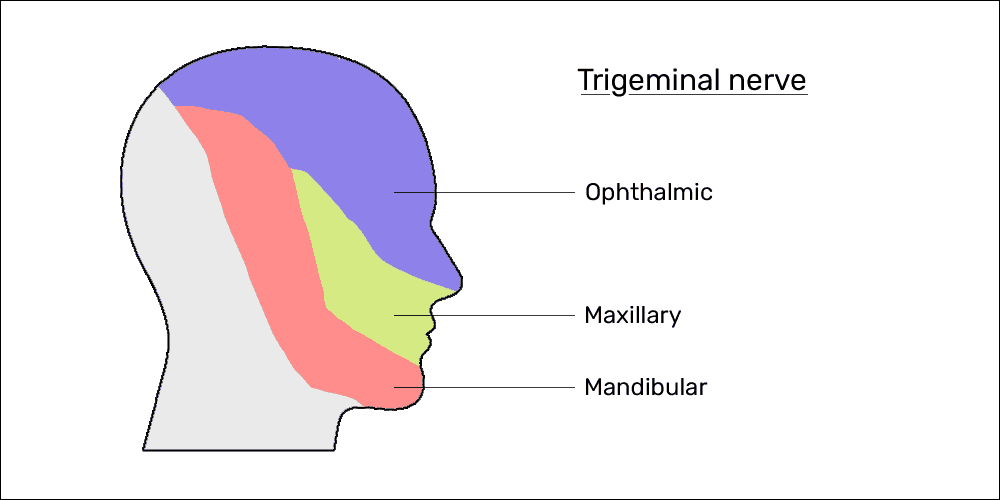
CSD involves a complex series of changes that lead to the release of neurotransmitter molecules (namely, potassium, nitric oxide, and adenosine) that irritate the trigeminal nerve endings surrounding the blood vessels in the meninges—the protective membrane that surrounds the brain and spinal cord.
More simply stated, the brain releases molecules that irritate its own protective sheath.
Phases of a migraine headache
Migraine headaches tend to have three phases. The first phase is called the prodrome phase, the second is the migraine or headache phase, and the third is called status migranosis.
- Phase 1: prodrome
- The pre-headache phase; patients will often recognize a migraine headache will occur, and an estimated 25% of migraine sufferers will experience a visual disturbance known as aura
- This phase will typically last approximately 30 minutes
- Phase 2: migraine headache phase
- The phase where the majority of symptoms will occur, classically including a debilitating headache
- This phase most often lasts a few hours; for the less fortunate, this may last longer than 24 hours
- Phase 3: status migranosis
- The final phase where the brain is attempting to recover; symptoms will usually persist but gradually decrease
- This phase may last 24-48 hours
Signs and symptoms
If you experience migraine headaches, you will likely experience different symptoms in each phase, and you may experience any combination of this long list of symptoms.
Phase 1: prodrome
Generally, patients describe feeling “uneasy” and can sense a migraine headache is on its way. In this phase, 25% of patients will experience aura—a visual disturbance that may include blurred vision, tunnel vision, or sharp blind spots.
Often times, the aura begins in peripheral vision and expands across the full field of vision. These visual disturbances will likely begin to fade and disappear after approximately 30 minutes
Phase 2: migraine headache phase
This phase is often characterized by a debilitating, pounding headache—often on only one side of the head. Along with this headache, common symptoms may include:
- Mild confusion
- Brain fog
- Nausea and vomiting
- Sensitivity to sound and light
- A sensation of numbness/tingling in specific areas of the body
- Feeling unsteady or unbalanced
- Short-term memory loss
- Difficulty with speech and/or language comprehension (including reading or writing)
Phase 3: status migranosis
The symptoms described in the migraine headache phase may persist for 24-48 hours after the onset. Generally, the symptoms will slowly improve until resolution.
Patients often describe this phase as “the migraine hangover,” comparing their symptoms to the way they feel after drinking alcohol.
Prevention and treatment
In our experience, patients have had decreased migraine frequency and decreased symptom severity with upper cervical spinal adjustments and manual therapy applied to the muscles of the head, neck, and upper back.
For migraine patients, we work with them to identify their triggers. We work together to create a log of their migraine headaches that includes:
- Time of day when the migraine began
- Physical location prior to and at the onset of the migraine
- Weather patterns in the day(s) leading to the migraine
- Food and drinks consumed in the days prior
- Daily physical and psychological stressors
- Mood and affect
- Recent sleep patterns
- Any changes in daily habits
Through this log, we work to identify and avoid potential triggers.
Additionally, we suggest supplementing caffeine (200-400mg for adults) daily to help prevent migraine headaches. Steady doses of caffeine, daily, may reduce the frequency and severity of migraine headaches with little-to-no associated risk.

For a migraine that has been triggered (e.g., the prodrome phase has begun), you may take an additional 200-400mg of caffeine. Research has indicated caffeine is an effective supplement to help reduce the duration and severity of migraine symptoms. The caffeine tends to be more effective the sooner it is taken following the onset of the prodrome phase.
Supplementing with oral cannabidiol (CBD) may also be effective for the prevention and/or treatment of migraine headaches. Check out our post on cannabis to learn more about the endocannabinoid system and how CBD helps to maintain homeostasis (balance for health and well-being) for all your cells and organ systems.
Note: since migraine headaches are neurological and non-inflammatory, using non-steroidal anti-inflammatory drugs such as Advil, Aleve, or Tylenol are not effective treatment options.
