Tendinopathy from gaming: eliminating the #1 career killing ailment
Key points
Disclaimer
This information is for educational purposes only and is not intended to replace the advice of your doctor. Esports Healthcare disclaims any liability for the decisions you make based on this information.
The information contained on this website does not establish, nor does it imply, doctor-patient relationship. Esports Healthcare does not offer this information for diagnostic purposes. A diagnosis must not be assumed based on the information provided.
Beyond eye strain and various postural issues, tendinopathy is among the most common ailments in gaming and esports. Defined as a painful, non-ruptured, non-inflammatory tendon ailment related to repetitive use, tendinopathy may occur in your shoulders, elbows/forearms, or wrists/hands.
However, despite having an infamous history for causing professional gamers to retire, there is wonderful news: tendinopathy is preventable! And, equally as wonderful, you can easily and successfully rehabilitate a tendinopathy with the Esports Healthcare tendinopathy treatment protocol.
Background of tendinopathy
Tendon pathology following repetitive physical use—and more specifically, in the absence of acute injury—has baffled many researchers and practitioners alike; both research and clinical treatment trends have added to the confusion with errors in nomenclature and the omission of extremely important, and seemingly simple, evidence-based details.
In this post, we will attempt to summarize clinical research about tendons, tendon injury, fascia, and treatment protocols to educate you on what we believe is the most efficient way to prevent and resolve tendinopathy.

The misnomer of “tendinitis”
Throughout the entire industry of healthcare—both in research and in practice—the term “tendinitis” has mistakenly been used to describe the painful, non-ruptured tendon ailments related to repetitive use. Even worse, the general public’s use of the word “tendinitis” is rampant and very rarely accurate.
However, in medical terminology, the suffix “-itis” is added to a word to identify inflammation as a major component of the pathology. Thus, the term tendinitis implies an inflammatory process involving a tendon structure.
In 1976, a researcher named Giancarlo Puddu discovered that inflammatory cells were not present in runners who experienced pain in their Achilles tendon absent of acute injury.1,2,3,4,5,6
And, despite this discovery and mountains of research that has followed, the term tendinitis continues to appear, inappropriately, in peer-reviewed research articles, published and recommended treatment protocols, and in discussion between providers and patients.
Why it matters
This misnomer is a serious problem! In fact, the treatment protocols are nearly the inverse of one another when considering a non-ruptured, inflammatory tendon ailment vs. a non-ruptured, non-inflammatory tendon ailment.
Generally, the recommendation for inflammatory ailments is, not surprisingly, anti-inflammatory measures including rest, cold and ice therapy, non-steroidal anti-inflammatory drugs (NSAIDs), and corticosteroids.
Unfortunately, none of these treatments would be beneficial—in the long-term—for a non-ruptured, non-inflammatory tendon ailment related to repetitive use!
Tendinopathy and the absence of inflammation
For the painful, non-ruptured, non-inflammatory tendon ailments related to repetitive use, the term tendinopathy should be used. This name implies pathology (disease or ailment) without implying the infiltration of inflammatory cells.
Thus, using the term “tendinopathy” allows for treatment protocols to be appropriately designed. Commonly, although not necessarily appropriate, these ailments are called overuse tendinopathy. We discuss why we believe this phrase is inappropriate in our Discussion, below.
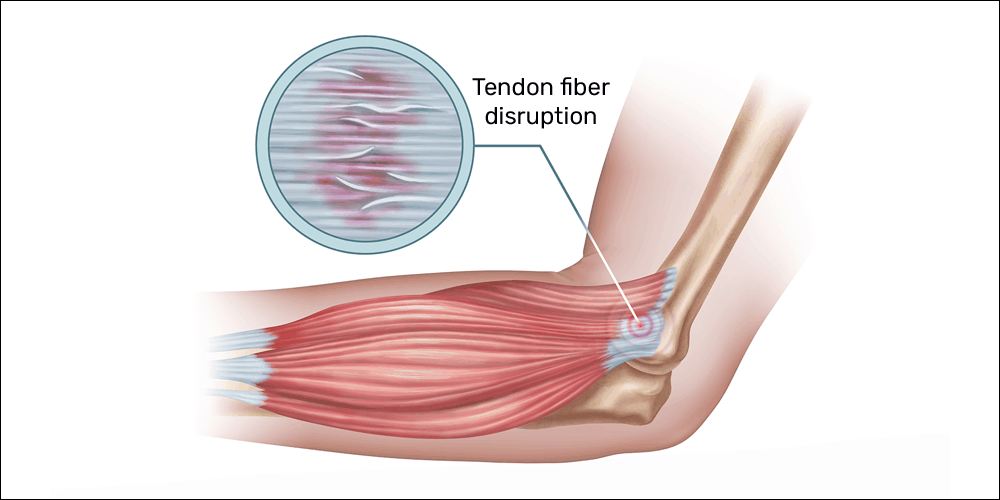
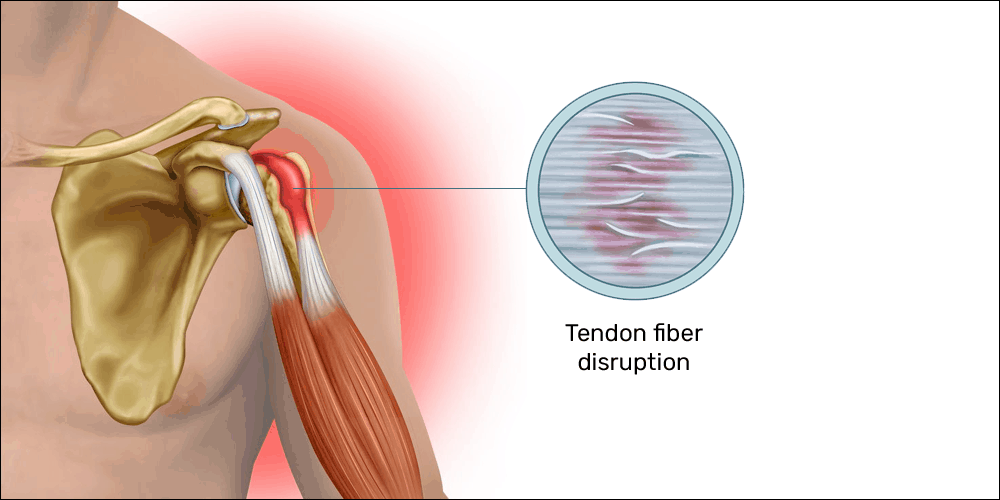
Histologically (at the cellular level), researchers have noted an absence of inflammatory cells. Inflammation is also absent in tendinopathy when viewed clinically (observed symptoms). According to Sharma and Maffulli,7
Histological examination of tendinopathy shows disordered, haphazard healing with an absence of inflammatory cells, a poor healing response, noninflammatory intratendinous collagen degeneration, fiber disorientation and thinning, hypercellularity, scattered vascular ingrowth, and increased interfibrillar glycosaminoglycans.
Sharma P, Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg Am. 2005;87:187-202.
Clinically, an inflammatory ailment would present, most often, as pain with accompanying redness, swelling, and heat (warm to the touch) when compared to other areas of the body. These three symptoms indicate the presence of increased blood flow. For tendinopathy, redness, swelling, and heat would not be observed.
Blood flow, or lack thereof, is likely one part of the issue of tendinopathy. Researchers often detail neovascularization (the formation of new blood vessels) in chronic tendinopathy that is not found in healthy tendons.7,8,9,10
Generally, neovascularization occurs when a tissue or group of cells need more blood to carry out their functions. This often happens following injury to assist in eliminating waste while also providing oxygen and nutrients—all of which are necessary for tissue repair.
Sharma and Maffulli describe tendon’s oxygen consumption as 7.5 times less than muscles—likely a result of anatomically limited blood flow—which helps to explain a slower recovery of tendons when compared to muscles.7
Mechanism of injury for tendinopathy
The mechanism of injury for tendinopathy from gaming is most often described as overuse. And, while this term is widely accepted, the ailments appear to be more related to movement imbalance. For example, a tendinopathy may not be related to excessive use but rather the use in an unfavorable body position and/or the absence of use in a particular phase or movement pattern.
The most common imbalance that leads to tendinopathy is concentric contraction without the counterbalance of appropriately loaded eccentric contraction:
- Concentric contraction: the shortening action of a muscle under tension
- Gaming examples: lifting your fingers off the mouse buttons; pressing console controller triggers or buttons
- Weight training examples – the up-phase of a biceps curl, bench press, or squat exercise
- Daily activity examples – pushing or pulling a door open
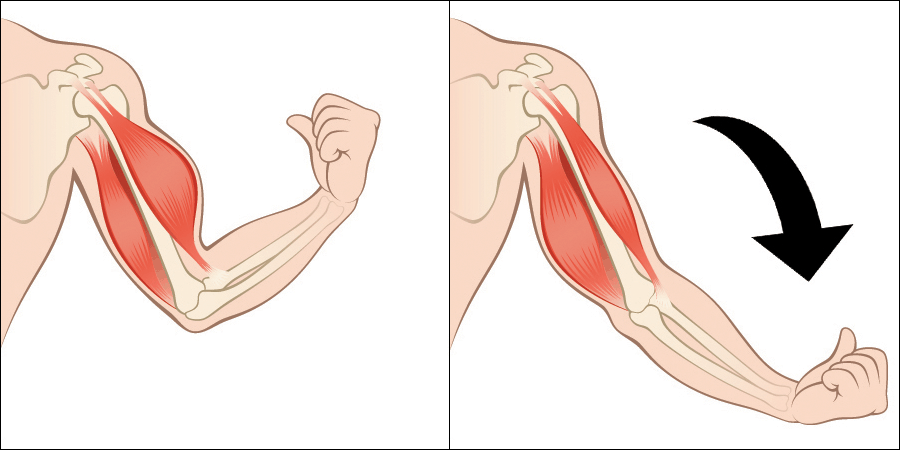
- Eccentric contraction: the lengthening action of a muscle under tension
- Gaming examples: none
- Weight training examples – the down-phase of a biceps curl, bench press, or squat exercise
- Daily activity examples – lowering a baby into a crib or putting a dog’s food bowl down
In this imbalance, the frequency of and/or resistance in the eccentric phase of muscle contraction is often significantly decreased or completely absent when compared to the frequency and/or resistance of its concentric counterpart.
Below are some common examples—both in and out of gaming—of concentric vs. eccentric imbalance:
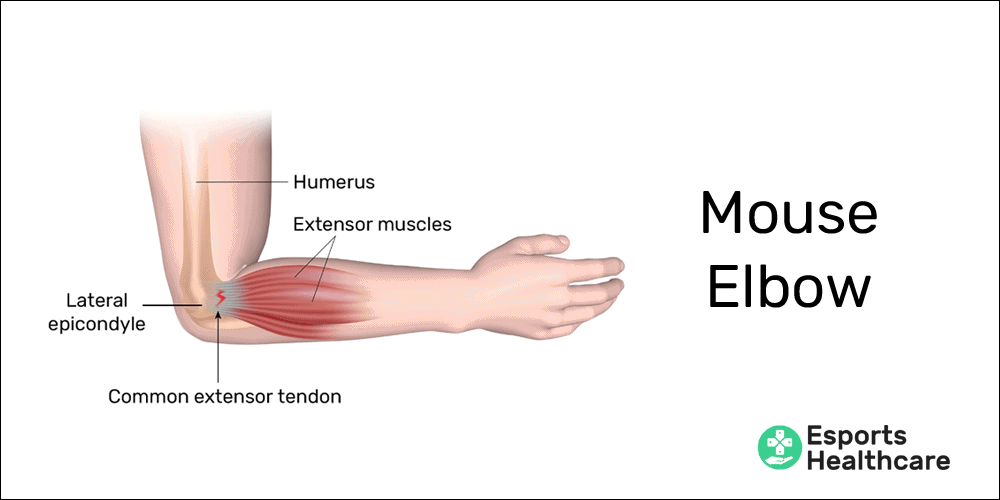
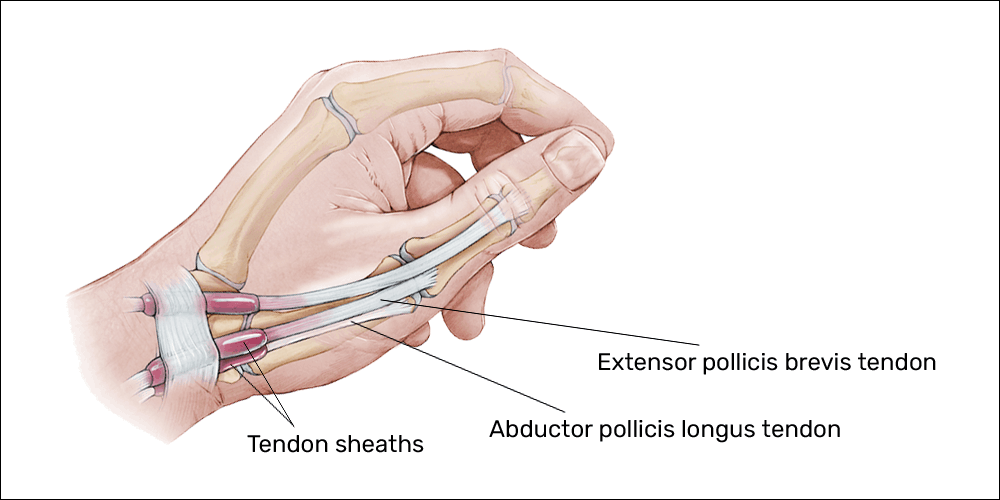
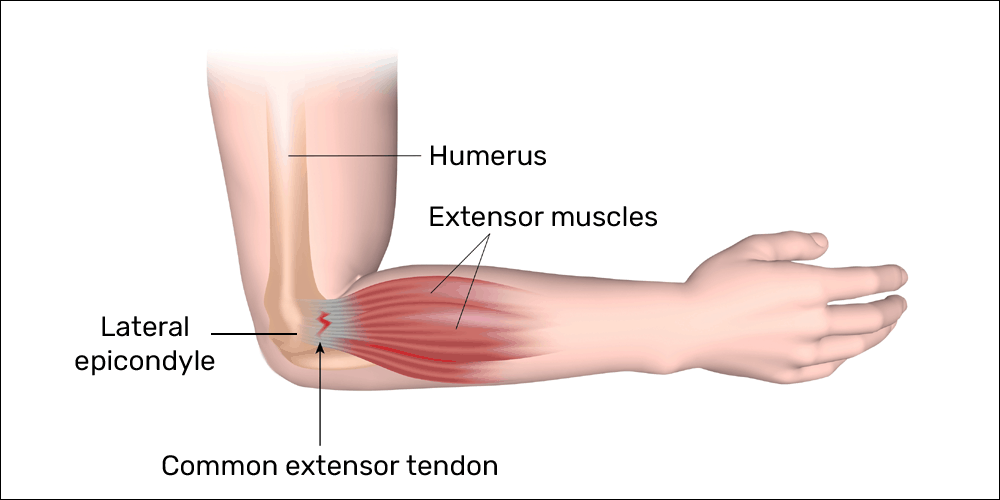
- Lateral epicondylosis (“mouse elbow”) in gamers and PC users
- Concentric action: lifting the fingers off the mouse and keyboard buttons; additionally, extension (bending back) and/or ulnar deviation (bending to the pinky side) of the wrist during keyboard and/or mouse use creates a shortening of the extensor muscles of the wrist (most notably, the extensor carpi ulnaris)—perpetuating concentric contraction
- Eccentric action: in PC use, there is no resisted eccentric phase of contraction for this muscle group
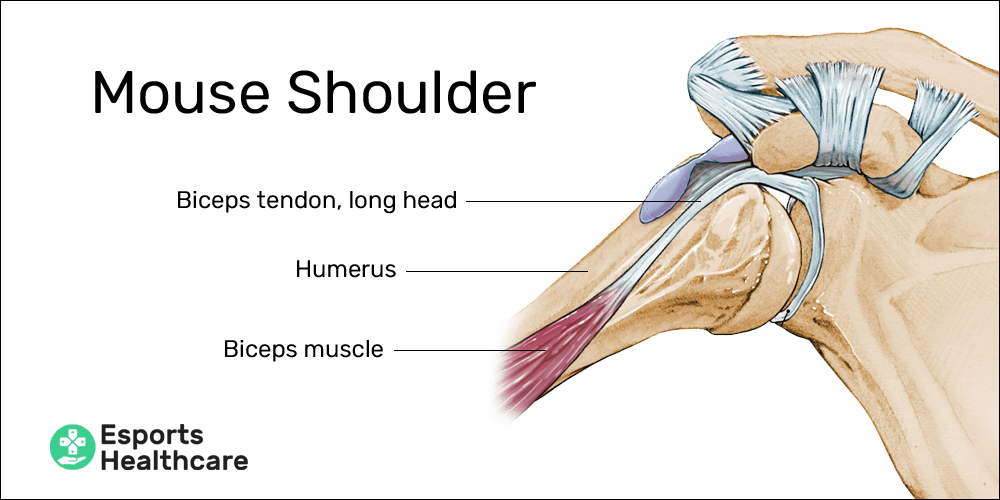
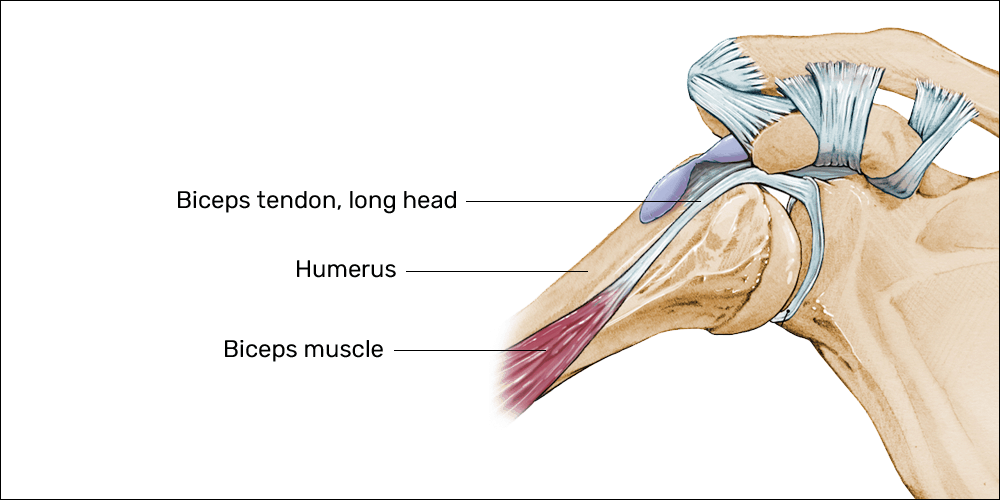
- Bicipital tendinopathy (“mouse shoulder”) in gamers PC users
- Concentric action: while using a PC, improper posture can create the need to reach for the mouse rather than allowing the arm to rest at the appropriate height; reaching out for the mouse creates a consistent concentric contraction of the biceps muscle with the greatest tension in the long head’s proximal attachment
- Eccentric action: in PC use, there is no resisted eccentric phase of contraction for this muscle
- Lateral epicondylosis (“tennis elbow”) in amateur tennis players
- Concentric action: backhand swings in amateur tennis players often include a “flick” (rapid extension) of the wrist—a concentric contraction of the extensor muscles and tendons of the wrist (which attach at the level of the elbow)
- Eccentric action: in this example, there is no eccentric phase of contraction for this muscle group while playing tennis
- Achilles tendinopathy in runners
- Concentric action: toe-off while running is a heavily resisted concentric contraction of the calf muscles (gastrocnemius and soleus) and Achilles tendon on every step while running
- Eccentric action: heel-striking or mid-foot striking limits the force and frequency of the eccentric component of the Achilles tendon via the calf muscles
A secondary imbalance—which ultimately leads back to the previous example of concentric without eccentric loading—is positional. If a movement pattern occurs in an unfavorable position, shortening of a specific muscle and its tendon may occur without appropriate lengthening.
The most common examples of this imbalance are noted in PC users
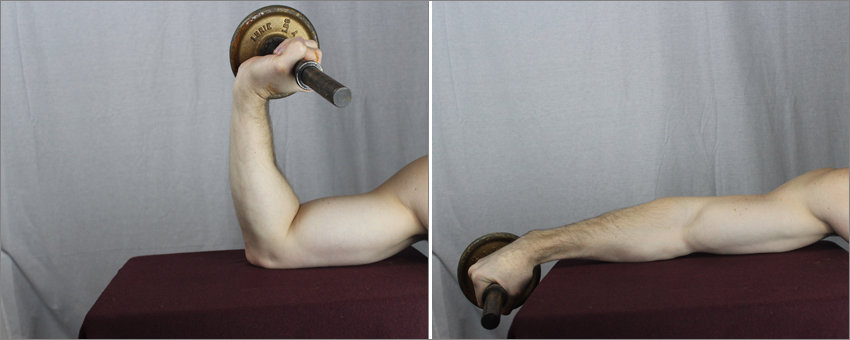
- Wrist extension: when using a keyboard and mouse, your wrists may be extended (bending backwards) due to the height of the equipment; your wrists should be straight to prevent excessive concentric action of the extensor muscles
- Radial/ulnar deviation: there may also be a tendency to have a bend in your wrist(s) either towards the thumb-side (radial deviation) or pinky-side (ulnar deviation—which is far more common); again, your wrists should be straight to prevent excessive concentric action of the extensor muscles

Ulnar deviation (bottom) is bending your wrist towards the pinky
Tendon anatomy
The simplest definition of a tendon is “the connective tissue attaching a muscle to a bone.” While this definition is easy to understand and provides enough information for the layperson, it is exceptionally insufficient to provide background that would help explain tendon pathology.
What you need to know
Tendons are bundles of parallel fibers that do, in fact, connect muscle to bone primarily consisting of type I collagen. Collagen is a protein that makes up approximately one-third of all proteins throughout your entire body. Collagen is found in bones, fascia (including tendons and ligaments), cartilage, and skin.
Additionally, tendons have some elastin (generally in the 1-2% range) which, as evidenced by its name, is a more elastic connective tissue that allows some pliability to certain tissues (e.g., fascia and skin).
Tendons are largely avascular, meaning the direct blood flow into the cells of the tendon matrix is limited or entirely absent. This is an important structural design to allow the strongest, uninterrupted structure possible.
Rather than having high volumes of blood, tendons have a ground substance (a gel-like material found between cells and tissues) mostly made of glycosaminoglycans (GAGs)—protein-sugar hybrid molecules that allow the tendon maintain fluid volume.
This ground substance has many roles which include providing nutrients, eliminating waste, and providing a lubricant for tissues that may be exposed to friction.
Fascia: the unsung hero of anatomy
Fascia is a broad category of connective tissue primarily involving collagen, elastin, and a ground substance consisting of proteoglycans/GAGs—most notably, hyaluronic acid.7,11,12,13 This definition should sound familiar to the description of tendon anatomy, above.
Fascia was defined at the first International Fascia Research Congress as:
The soft-tissue component of the connective tissue system that permeates the human body, forming a whole-body continuous three-dimensional matrix of structural support. It interpenetrates and surrounds all organs, muscles, bones and nerve fibers, creating a unique environment for body systems functioning.
Fascia can refer to dense planar fascial sheets (such as the fascia lata) as well as joint capsules, organ capsules, muscular septa, ligaments, retinacula, aponeuroses, tendons, myofascia, neurofascia, and other fibrous collagenous tissues.
More recently, at the fourth International Fascia Research Congress (2015), two definitions were proposed: 11
Fascia is “a sheath, a sheet, or any other dissectible aggregations of connective tissue that forms beneath the skin to attach, enclose, and separate muscles and other internal organs.”
The fascial system “consists of the three-dimensional continuum of soft, collagen-containing, loose and dense fibrous connective tissues that permeate the body, providing an environment that enables all body systems to operate in an integrated manner.”
For tendinopathy treatment design, the most important aspect of these definitions is the inclusion of tendons as a sub-category of fascia. Since tendons are bundles of fascia, tendons can and should be treated in a similar fashion as fascia.
Signs and symptoms
If you’re affected by tendinopathy, you’re likely to experience the following symptoms:
- Pain along the tendon in question
- A tendinopathy will be more painful when you put pressure on it (e.g., massaging the tendon)
- Increased pain when the muscle/tendon contracts, both in concentric and eccentric phases
- Increased pain when the muscle/tendon is stretched (e.g., stretch and hold positions)
- Perceived weakness
- A tendinopathy will cause perceived weakness; in other words, the muscle and tendon can manage a normal resistance, but the pain will likely inhibit your desire to fully contract the target muscle
Other common findings may include:
- More pronounced symptoms during your gaming sessions
- Worsening symptoms following periods of rest
- Relief or improvement of symptoms after warming up
Note: in a tendinopathy, inflammation will not be present. Inflammation is categorized by pain with accompanying swelling, redness, and heat (feeling warm to the touch).
If you notice these signs of inflammation, you are likely experiencing something different than simple tendinopathy. You should consult your doctor if you are concerned about these symptoms.
Considerations for tendinopathy
Some important details in the effective treatment of tendinopathy are as follows:
Common mechanism(s) of injury
Movement imbalance: tendinopathy is most often a result of movement imbalance—primarily, a lack or absence of eccentric contraction and/or insufficient resistance in the eccentric phase—as described above.
Acute trauma: tendinopathy may also follow acute trauma (e.g., acute strain injury); however, the underlying issue is likely, again, immobility or lack of appropriate movement (properly loaded eccentric phase) during recovery.1,2,7,13
Tendons are a sub-type of fascia
Since tendons are bands of fascia, they will undergo physical changes—identified as haphazard healing and adhesion/densification formation—following chronic movement imbalance or acute injury followed by inappropriate recovery techniques.7,13
Blood flow to tendons is limited
There is significantly less blood flow in tendons when compared to muscles. Rather, tendons receive nutrients from their ground substance of proteoglycans/glycosaminoglycans (hyaluronic acid).7,11,12,13
Mechanical loading promotes healing
Mechanical loading (appropriately loaded physical strain) on a tendon aids to increase DNA content and promote protein synthesis of the tenocytes (tendon cells); loading in eccentric also aids to improve tendon fiber alignment.7,12,13
Preventing tendinopathy
Since tendinopathy is caused by movement imbalance, the prevention—in theory—is rather simple: maintain movement balance.
Granted, in real life gaming situations, this notion is not always simple. The good news, though, is that you do not necessarily have to be perfect 100% of the time while you’re gaming. Instead, you can perform exercises prior to and following your gaming sessions to effectively limit your risk of developing a tendon pathology.
Four steps to prevention
Step 1: warm-up
Prior to gaming, warm-up the muscles, tendons, and joints that will be used during your session. For this exact purpose, we’ve created a gamer warm-up—a comprehensive routine to include all muscles, tendons, and joints utilized in all gaming sessions including your eye muscles!
Step 2: posture and ergonomics
Correct and maintain appropriate body positions while gaming. This includes your whole body posture as well as hand and wrist positioning.
Recall from the section on Mechanism of injury above, we explain wrist extension (bending backwards) and radial/ulnar deviation (side-to-side bending) of the wrist will exacerbate movement imbalance, especially for PC gamers.
Step 3: stretch
After you’re done with your gaming session for the day, stretch your muscles and tendons. Also for this exact purpose, we’ve created a routine of gamer stretches—a comprehensive routine to include all the same muscles and tendons utilized in all gaming sessions.
Step 4: therapeutic exercises
Perform resisted exercises to challenge the tendons that are chronically shortened during gaming sessions. Again, we’ve created a video routine for this exact purpose. This injury prevention routine includes therapeutic resistance exercises and stretches to reverse the potential harm accumulated during gaming sessions.
For this routine, we recommend performing these exercises according to your weekly gaming volume. For example, if you play video games 1-2 days per week, performing this routine once per week should be sufficient.
If you play 3-4 days per week, performing this routine twice per week would be more appropriate. And, if you’re gaming 5-7 days per week, we recommend performing this routine 3 times per week.
Addressing tendinopathy considerations
Identify and correct movement imbalance(s)
The most common mechanism of injury for tendinopathy from gaming is movement imbalance. Any/all treatments will be ineffective if the movement imbalance persists throughout the duration of the treatment protocol. The most important step is to identify and correct any imbalance(s)!
Fascial manipulation
Appropriately targeted, aggressive cross friction (fascial manipulation) assists in breaking apart adhesion/densification formation within the tendon matrix.12,13

Note: for more information, see Fascial Manipulation® Method by Luigi Stecco, PT; Carla Stecco, MD PhD; Antonio Stecco, MD PhD; and Warren Hammer, DC
Promote blood perfusion
Blood flow to any tissue is important to assist in removal of debris as well as to bring oxygen and nutrients to the healing tendon. Therefore, use of anti-inflammatory measures—namely, ice, NSAIDs, and corticosteroids—may further decrease the volume of blood that reaches the ailing tendon.
Instead, it is important to promote blood perfusion to the target tendon in an attempt to more rapidly remove any debris while providing oxygen and nutrients necessary for healing.
Perform heavily resisted, eccentric contractions of the injured tendon
The most common mechanism for tendinopathy from gaming is movement imbalance including a lack of or complete absence of eccentric loading. Performing heavily resisted, eccentric contractions on the injured tendon will combat this movement imbalance while promoting DNA content and protein synthesis (in other words, healing) of the injured tendon.
Treatment protocol for tendinopathy
I created this protocol from a combination of: research on the anatomy, physiology, and pathophysiology of both fascia and tendons; research on the clinical trends for treatment of both tendinopathy and fascial adhesions; and years of experience treating tendon and fascial ailments including both successful and less-successful treatment plans.
In my latest experience treating tendinopathies in the second half of 2020, I utilized the protocol described below which was successful in resolving pain and dysfunction in 5 different patients with 5 different tendinopathies—all in 3-5 visits.
Corey J. Csakai, DC – Owner of Esports Healthcare
In private practice, all patients diagnosed with tendinopathy—regardless of the location—were treated with the following protocol:
Step 1: fascial manipulation
To begin, the provider should perform ~10 minutes of fascial manipulation (or equally aggressive, cross-friction manual therapy) to the site of the affected tendon where adhesion/densification formation is noted.
This technique is often extremely painful for the patient. Treatment should be dosed to patient tolerance; patient must be instructed to stop the provider when the pain feels too severe! The provider should attempt to accumulate ~10 minutes of total treatment time or until pain from treatment resolves.
Note: for more information, see Fascial Manipulation® Method by Luigi Stecco, PT; Carla Stecco, MD PhD; Antonio Stecco, MD PhD; and Warren Hammer, DC
Step 2: promote blood perfusion
For our case reports, we performed ~10 minutes percussion massage using the Hyperice® Hypervolt+® to the affected tendon and surrounding soft tissue.
For example, Achilles tendinopathy would include the heel of the foot, the calf muscles, and the Achilles tendon. Biceps tendinopathy would include the deltoid (anterior and lateral portions, specifically), the biceps muscle bellies, and the proximal, long head tendon.
For our purposes, we used percussion massage with the specific goal of stimulating blood flow. Following ~10 minutes of the Hypervolt+, the skin in the area was red and warm to the touch—a clinical indication of increased blood flow.
Because all our case reports received the Hypervolt+ for this step, we are unable to identify whether or not other heat modalities would be equally as effective. The percussion massage may be promoting further healing beyond improving blood perfusion to the target tendon; without histologic testing, we cannot appropriately make this determination.
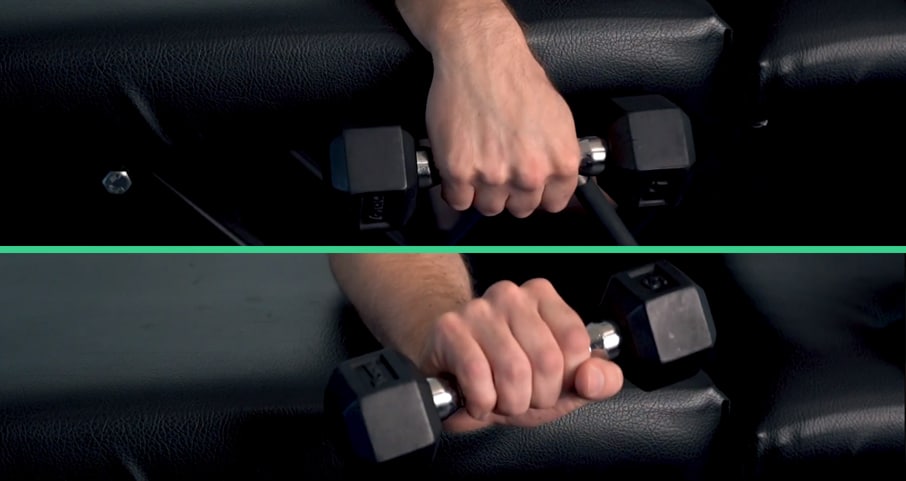
Step 3: heavy, eccentric loading
Following increased blood flow to the area, the patient should then perform 3 sets, 8-10 repetitions of heavy, eccentric loading on the affected tendon.
To do so, the target muscle/tendon should be shortened as much as possible (without adding resistance in the concentric phase). Then, adding as much resistance as the patient can manage, allow the muscle/tendon to lengthen to a stretched position.
In private practice experience, the first set was often described as “moderately painful,” the second set was often described as “uncomfortable,” and the third often resulted in fatigue with a noticeable decrease in pain.
For our case reports, the patients were instructed to resist as strongly as possible, and the provider created enough resistance to initiate movement—approximately 3 seconds per repetition, eccentric-only.
Step 4: continue to promote blood perfusion
Patients were all instructed to continue use of heat therapies at home (e.g., either dry or moist heat packs) and were specifically instructed to avoid use of ice, NSAIDs, or other anti-inflammatory measures.
Further discussion
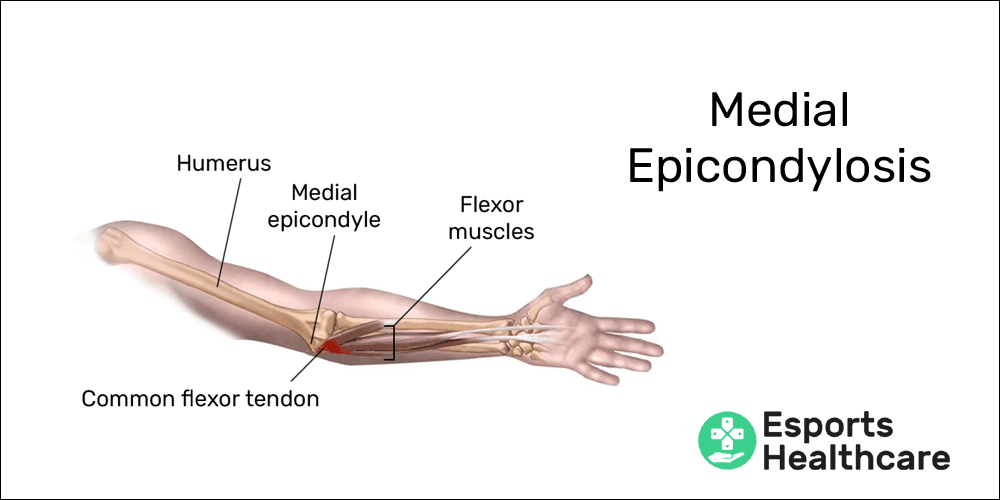
Tendinopathies are among the most common ailments that gamers may face in their careers. In our injury library, we’ve already created pages for three common tendinopathies: mouse elbow, mouse shoulder, and medial epicondylosis.
Many health care providers and non-medical personnel alike will describe these ailments using the terms “overuse.” While this term is not entirely inaccurate, it is not specific to the real cause of tendinopathies.
Overuse strains
Acute overuse strains are common injuries when someone performs too many actions in a short period of time for which their muscles are not accustomed. In the winter, shoveling snow is a common cause for acute overuse strains.
After a workout or aggressive activity, delayed-onset muscle soreness should last no more than 2-3 days. In an acute overuse strain—short of a rupture (a torn muscle)—these ailments usually present with muscle spasm and severe pain/soreness for more than 3 days.
For the acute overuse injury, the ailment generally occurs in the muscle—the microscopic fibers of the muscle are broken down due to excessive volume of contraction and usually against a greater-than-normal resistance. In this situation, the tendons are usually not affected.
However, if the tendon is involved, this is when the term tendinitis is appropriate! Following acute strain, inflammation will occur in a tendon, but this is not the ailment that occurs as a result of playing video games.
As described earlier, the reason for the prevalence of tendinopathies in gaming is movement imbalance. Most gaming movements are concentric in nature, and eccentric movements are virtually non-existent.
References
- Khan K, Cook J. The painful nonruptured tendon: clinical aspects. Clinics in Sports Medicine. 2003:711-25.
- Astrom M, Rausing A. Chronic Achilles tendinopathy. A survey of surgical and histopathologic findings. Clin Orthop. 1995;316:151–64.
- Khan KM, Cook JL, Bonar F, Harcourt P, Astrom M. Histopathology of common overuse tendon conditions: update and implications for clinical management. Sports Med 1999;27:393–408.
- Khan KM, Cook J, Kannus P, Maffulli N, Bonar S. Time to abandon the ‘tendinitis’ myth. BMJ. 2002;324:626–7.
- Cook JL, Khan KM, Maffulli N, Purdam C. Overuse tendinosis, not tendinitis: part 2. Applying the new approach to patellar tendinopathy. PSM. 2000;28(6):31–46.
- Alfredson H, Lorentzon R. Chronic Achilles tendinosis: recommendations for treatment and prevention. Sports Med. 2000;29(2):135–46.
- Sharma P, Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg Am. 2005;87:187-202.
- Natsu-ume T, Nakamura N, Shino K, Toritsuka Y, Horibe S, Ochi T. Temporal and spatial expression of transforming growth factor-beta in the healing patellar ligament of the rat. J Orthop Res. 1997;15:837-43.
- Marui T, Niyibizi C, Georgescu HI, Cao M, Kavalkovich KW, Levine RE, Woo SL. Effect of growth factors on matrix synthesis by ligament fibroblasts. J Orthop Res. 1997;15:18-23.
- Ohberg L, Lorentzon R, Alfredson H. Neovascularisation in Achilles tendons with painful tendinosis but not in normal tendons: an ultrasonographic investigation. Knee Surg Sports Traumatol Arthrosc 2001;9(4):233–8.
- Fede C , Pirri C, Fan C, Petrelli L, Guidolin D, De Caro R, Stecco C. A Closer Look at the Cellular and Molecular Components of the Deep/Muscular Fasciae. Int J of Mol Sci. 2021;22(3):1411.
- Findley T, Chaudhry H, Stecco A, Roman M. Fascia research – a narrative review. J of Body & Move Ther. 2012;16(1):67-75.
- Pavan PG, Stecco A, Stern R, Stecco C. Painful connections: densification versus fibrosis of fascia. Curr Pain Headache Rep. 2014;18(8):441.